ROUX-EN-Y Gastric Bypass – On the way to Weight Loss
First and foremost, the treatment of obesity focuses on a conservative approach. Doctors, dieticians, psychologists, psychotherapists and physiotherapists are involved in this method. If this approach is not sufficient to achieve sufficient weight loss, a surgical procedure is considered if the body mass index (BMI) is over 40 or – if concomitant diseases are present – a BMI of over 35. BMI – also body mass index, body mass number or Quetelet-Kaup index – is a measure for evaluating a person’s body weight in relation to their height. The BMI is calculated by dividing the body weight in kilograms by the height in meters squared. As BMI, or obesity, increases, the risk of obesity-related diseases increases.
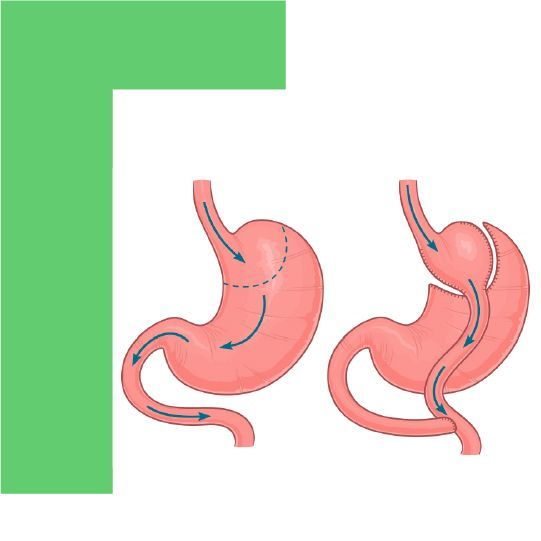
The surgical procedures used in obesity therapy are “restrictive” and “malabsorptive” procedures. Restrictive procedures, like tube stomach surgery, involve the sole reduction of the amount of food that can be fed by reducing the volume of the stomach. Malabsorption is the reduction of food intake from the food pulp by eliminating a segment of the small intestine of varying length. Gastric Bypass surgery is a predominantly restrictive procedure with concomitant malabsorptive effects. In contrast, the variant, omega-loop Roux-En-Y Gastric Bypass surgery, focuses on malabsorption. Both Gastric Bypass procedures are reversible. The original anatomy can be restored because no parts of the intestine and/or stomach are removed.
Patients must understand their role
Gastric Bypass surgery is recommended for patients with a BMI greater than 40 or with a BMI between 35 and 40 in the presence of associated comorbidities when conservative attempts at weight loss have already failed. Gastric surgery is not recommended in cases where severe concomitant diseases increase the risk of surgery. Also in adolescents, Gastric Bypass is considered only in exceptional cases, especially if the development is not yet complete. In older patients, the decision is made individually. In any case, it is important that the patient cooperates well and understands the therapy in order to achieve the surgically supported therapeutic goal – weight reduction.
Performing Gastric Bypass
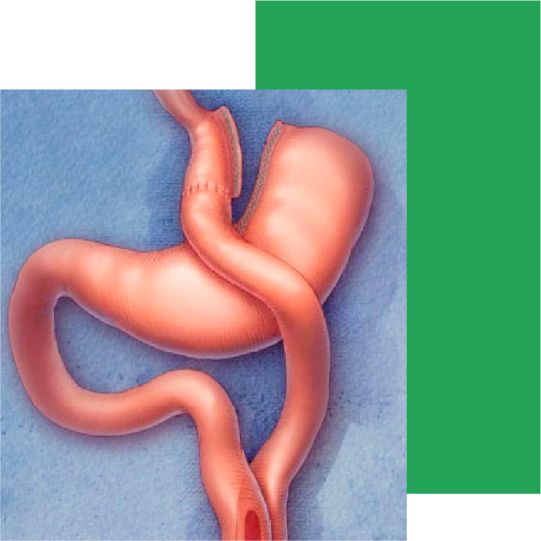
Both forms of Gastric Bypass are performed in Turkey using minimally invasive surgery. The patient is quickly mobilized and scarring is minimal. The patient can leave the hospital after 3 to 6 days. In Gastric Bypass surgery, the amount of food that can be fed is considerably reduced by reducing the size of the stomach. The altered anatomy after the surgery, but also the altered flow of the food pulp, lead to a change in various hormones of the gastrointestinal tract that are responsible for satiety and hunger.
Performing Gastric Bypass
Both forms of Gastric Bypass are performed in Turkey using minimally invasive surgery. The patient is quickly mobilized and scarring is minimal. The patient can leave the hospital after 3 to 6 days. In Gastric Bypass surgery, the amount of food that can be fed is considerably reduced by reducing the size of the stomach. The altered anatomy after the surgery, but also the altered flow of the food pulp, lead to a change in various hormones of the gastrointestinal tract that are responsible for satiety and hunger.
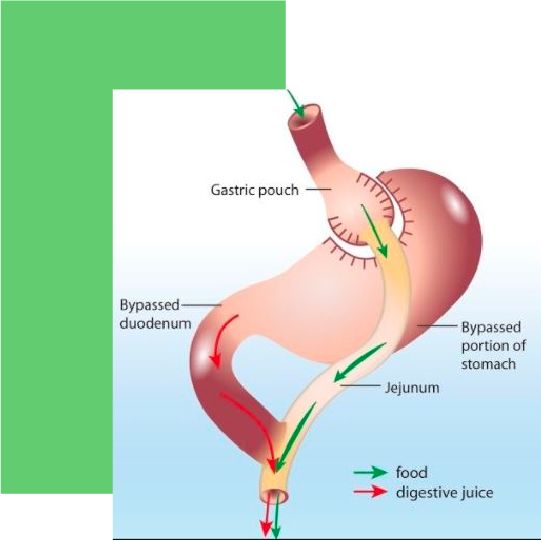
During the surgery, a part of the stomach is first separated from the stomach directly following the transition of the esophagus into the stomach. This small stomach pouch still allows food to flow. The rest of the stomach remains in the abdominal cavity. The small intestine is then cut about 50 to 150 cm after the duodenum, and the lower portion near the large intestine is connected to the gastric pouch. The small intestine portion coming from the rest of the stomach is sutured into the small intestine leg coming from the stomach about 150 to 50 cm after the stomach-small intestine connection. The digestive enzymes coming from the liver, pancreas and stomach are thus added to the food pulp. The mix of digestive enzymes and food mush leads back to normal digestion of the food mush.
The Positive Changes
Relative to other surgical interventions for obesity, Roux-En-Y Gastric Bypass results in the most stable and, most importantly, long-term weight loss effects. Within 12 to 24 months, weight loss averages 80 percent of excess weight. This generally results in a serious decrease in secondary diseases. Studies show that blood glucose levels in type 2 diabetes mellitus sometimes return to completely normal after surgery. Blood pressure and blood lipid levels drop. Consequently, the risk of heart attack also drops sharply. Above all, however, there is a demonstrable increase in self-esteem and, as a result of all these changes, an improvement in general health.
However, the success of the surgical intervention is strongly dependent on postoperative behavioral patterns of the patient. For example, weight loss with its positive consequences can be stabilized by avoiding high-calorie drinks and food in porridge form. Otherwise, the same amount of calories as before bypass may enter the body, thereby supporting weight gain.
Negative consequences
Postoperative complications may occur in approximately 15-18% of cases. These include simple bleeding from skin incisions, inflammation, or scar fractures, which can occur with all abdominal surgeries. In a condition called dumping syndrome, surgery may bypass a layer of muscle normally located at the stomach outlet that prevents food from passing quickly into the small intestine. Rapid passage of the food pulp into the small intestine may occur, resulting in nausea and bloating. In addition, the inadequately predigested food pulp deprives the body of fluids, which can result in circulatory collapse.
This is especially the case with dairy products and high-carbohydrate foods. In addition, hypoglycemia can occur a few hours after food intake. Since sugar is absorbed very quickly into the body via the intestines, the blood sugar level drops rapidly due to the release of insulin. To prevent this, it is advisable to eat small meals more frequently.
Stomach acid or bile can flow back into the esophagus from the reduced stomach, which can lead to heartburn or inflammation of the esophagus. Good chewing, small meals and avoiding carbonated beverages reduces the risk of these complaints. However, cosmetic problems may also arise. Successful weight loss can result in the formation of skin flaps, especially on the abdomen, arms, thighs and chest. These skin flaps may necessitate cosmetic surgery, which makes sense because fungal infections of the skin often occur between the skin flaps.
And people with Gastric Bypass should avoid alcohol as far as possible or consume it only in very small quantities, because the smaller stomach means that a higher alcohol level is reached more quickly.
Advantages and Disadvantages of Gastric Bypass
Advantages
– Roux-En-Y Gastric Bypass is a limited procedure. It is not very aggressive and is reversible.
– It is the most commonly performed weight loss procedure.
– Gastric Bypass is considered the gold standard surgery for reliable weight loss.
– Long-term results show an average weight loss of 60% to 70%.
– Many health problems such as sleep apnea, gastroesophageal reflux, heartburn, incontinence and respiratory function are resolved.
– Risk of heart attack decreases
– Minimum 60% of hypertension patients no longer need medication.
Roux-En-Y Gastric Bypass surgery is recommended as a safe therapy for elderly or cardiac patients. Short postoperative pain, short time in the hospital, quick return to daily life and a very small rate of wound infections.
Disadvantages
– Most bariatric patients already have comorbidities that increase the risk of further complications.
– Cardiopulmonary and wound-related complications lead to most cardiovascular accidents.
– Circa 10% of all patients have postoperative complications due to deficiencies of folic acid, thiamine, calcium, zinc, vitamin B12, vitamin D, vitamin A, and iron. This can lead to anemia, encephalopathy, and other conditions.
– Patients with addictive behaviors often cannot adhere to diets and medical instructions, so there is little weight loss and the risk of complications is especially high.
– Patients with food addictions may transfer that addiction to drugs or alcohol after surgery. All of this can lead to weight gain and further rework.







